By Bob Aller
Posted December 2, 2024
Reckless, Persistent Disregard For ER Patient Safety By Kaiser Administrators
Kaiser ER nurse understaffing caused the horrific death of a 53-year-old father of four, Francisco Delgadilla-Machuca. It happened in the ER waiting room of Kaiser Permanente’s Vallejo Medical Center. According to nursing staff, years of flagrant understaffing set the stage for this inevitable tragedy. A CMS investigation revealed layers of troubling facts in a February 7, 2024, Summary Statement of Deficiencies.

Kay Facts |
|
| Patient | Francisco Delgadilla-Machuca, 53 |
| Incident Date | December 8, 2023 |
| ER Waiting Room | Kaiser Permanente Vallejo Medical Center, California |
| Triage Classification | Emergency Severity Index (ESI) Level 2 – minimum reassessment every 2 hours |
| Time of Arrival | 3:45 p.m. |
| Time of Death | 11:59 p.m. |
| Autopsy Report | Ruptured thoracic aortic aneurysm |
| CMS Finding | Inadequate staffing and failure to monitor waiting-room patients |
| Prior Citation | CMS deficiency report, 2021 – delayed triage at the same facility |
Staffing Complaints With Legal Implications Ignored!
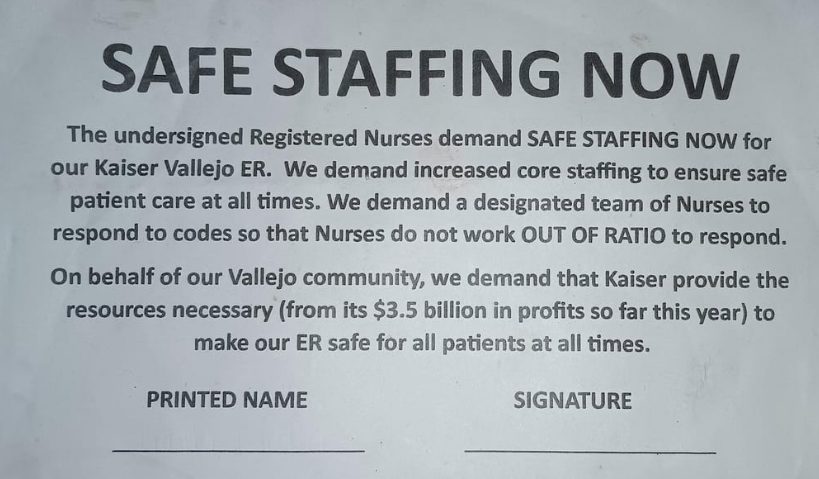
Kaiser Vallejo ER nurses repeatedly protested understaffing at the hospital’s 52-bed emergency department, documenting conditions on Assignment Despite Objection (ADO) forms. The ADO is a legal notice in which a nurse states that an assignment is unsafe and places patients at risk, while agreeing to proceed under protest in accordance with the California Nursing Practice Act.
“As a patient advocate… today’s assignment is unsafe and places my patients at risk. As a result, the facility is responsible for any adverse effects on patient care. I will, under protest, attempt to carry out the assignment to the best of my ability.”
Nurses cited recurring unsafe conditions, including:
- Unanswered call lights.
- Delays in medication administration.
- Required staffing ratios not met.
- No triage at times.
- Nurses are leaving assigned patients to assist elsewhere.
Despite multiple documented incidents tied to staffing levels, administrators did not implement corrective staffing to address the ER’s ongoing monitoring and coverage gaps.
Preventable Tragedy Unfolds
On December 8, 2023, while at work, Francisco Delgadilla-Machuca developed severe chest and back pain and drove ~30 miles to the Kaiser Permanente Vallejo ER.
He arrived at 3:45 p.m. PT, and the medical team triaged him immediately. He described sharp chest pain rated 7 out of 10, while his blood pressure read 170 over 85 mmHg. As a result, doctors identified it as a possible cardiovascular emergency and prepared for urgent care.
The triage nurse assigned him an Emergency Severity Index (ESI) Level 2, which requires frequent checks of his condition and vital signs per facility policy and CMS regulations. However, CMS later reported that staff failed to perform any such monitoring in the waiting area. At the time, reportedly 30 to 40 patients were in the waiting room. However, no nurse was designated to monitor patients.
Family’s Desperation Call to 911
As Francisco’s pain intensified around 5:00 p.m., his family feared he would die without treatment. A family member stepped outside the Kaiser Vallejo ER at 5:14 p.m. and called 911, pleading for an ambulance to transfer him to another hospital.
A fire engine arrived within six minutes. According to family accounts and the responding team, the lead EMT explained to the family, including Francisco in a wheelchair, that once a patient is registered at Kaiser, the fire department cannot transport the patient elsewhere. The EMT then went inside and spoke with the admitting clerk. Shortly after, Francisco was taken into the ER, where staff documented pain at a level 10.
Per Kaiser pain-scale materials, a score of 10 represents “the worst pain possible” and warrants immediate medical evaluation. Records showed that no physician evaluation was conducted.
Francisco was returned to the waiting room, which was not being monitored, and remained there about six more hours until his collapse around 11:30 p.m. PT. He was pronounced dead at 11:59 p.m. by Dr. Nisha Chauhan.
Son & Family Witnessed Francisco’s Decline In the ER Waiting Room
Francisco’s son, Francisco Luz De Leon, commented:
“He held his shirt over his heart… he couldn’t sit still… he ended up lying on the floor.”
The waiting room was crowded, yet his father appeared more distressed than anyone nearby.
- Guarding the chest: holding his shirt where his heart was
- Visible agitation: struggling to sit; shifting constantly
- Functional decline: eventually lying on the floor due to pain/distress
De Leon asked the ER admitting clerk when his father would receive care. According to the family, the clerk said there were ~28 patients ahead. As Francisco’s condition worsened, additional family members arrived and watched other patients being taken inside for immediate treatment, while Francisco was left in the waiting area.
Francisco Collapses Onto ER Waiting Room Floor
Around 11:30 p.m. PT, Francisco’s son spoke with a newly arrived admitting clerk, who said his father was fifth in line. “We were all glad, relieved,” he recalled. “But it was too late. I saw my father collapse. I ran to support him and heard his last breath.”

Francisco’s wife, Maria, recalled that terrible moment: “I turned around, and that’s when my husband fell to his knees and went out on the floor. He was just five numbers away from his turn. I went crazy yelling at all the doctors, kicking the trash cans, and throwing water bottles.”
Francisco lay on the waiting-room floor, surrounded by family. Records indicate that no physician evaluation was documented for approximately eight hours before the collapse. Dr. Nisha Chauhan then evaluated him; resuscitation attempts failed, and Dr. Chauhan pronounced him dead at 11:59 p.m. PT.
The family requested several hours to grieve. Afterward, Francisco’s remains were transported to the county morgue.
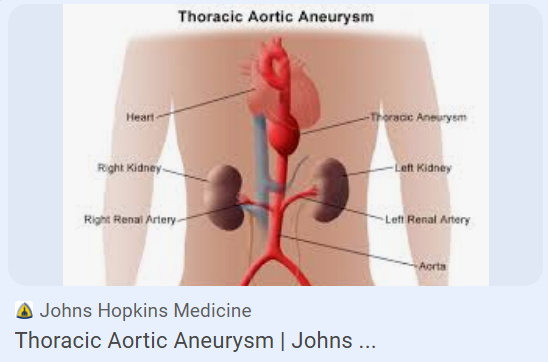
Autopsy: Ruptured Thoracic Aortic Aneurysm (TAA)
On the morning of December 11, 2023, a forensic pathologist at the Solano County Coroner’s Office conducted the autopsy.
 Autopsy Findings:
Autopsy Findings:
The autopsy determined that Francisco Delgadilla-Machuca died from a ruptured thoracic aortic aneurysm (TAA). This was a catastrophic tear of the thoracic aorta, causing massive internal hemorrhage.
He bled out. This event is considered extremely painful, like a “severe, tearing pain in the chest or upper back.” The tearing can be all at once, or it can extend over time as three layers of tissue tear. With the rupture, blood pressure finally falls precipitously, leading to a state of shock. This event causes about 30,000 deaths a year in the U.S.
Francisco’s four sons and his wife were present in the Kaiser Vallejo ER waiting room when he collapsed. Chronic understaffing and the lack of waiting-room monitoring led to his death.
Long Waits Were Not Unusual at Kaiser Vallejo ER

After the Feb. 7, 2024, CMS deficiency summary was released, NBC investigative reporter Hilda Gutierrez covered the case. She interviewed Raquel Benito, RN, the California Nurses Association representative for Kaiser Vallejo ER nurses. According to Benito:
- An 8-12 hour wait for patients was not unusual.
- The ER was operating with ~6 nurses on duty, less than half of the ~14 nurses needed for the unit.
- For years, understaffing was an issue. Management continuously ignored complaints of inadequate staffing.
CMS Previously Cited Kaiser ER for Understaffing (2021)
According to CMS records, an EMT complaint in 2021 triggered a Summary Statement of Deficiencies at the Kaiser Permanente Vallejo ER. In interviews, multiple ER staff members described persistent understaffing.
Failure to Provide Timely Triage (EMTALA)
This CMS report found that understaffing at Kaiser’s Vallejo ER caused serious delays in triages. EMTALA was violated by failing to provide a timely triage for patients.
- Ambulance arrivals: EMS crews reported standing by with patients on gurneys for extended periods due to a lack of available triage capacity.
- Clinical impact: According to CMS, the patients suffered deteriorating conditions.
Delayed 911 Turnaround
The report described four cases where ambulances waited over an hour before the patients were seen. The ambulance crews could not leave until their patients were admitted. Thus, the Kaiser Vallejo ER caused improper delays in the community’s 911 medical response times. Those delays adversely impacted patients waiting for an ambulance after suffering from heart attacks, strokes, other critical conditions, or accidents.
No Staffing Increase Following the 2021 Deficiency Report
The ER’s Director, Nurse Practitioner Daphne Morris, stated that after the 2021 CMS report, Kaiser did not increase core nurse staffing. She requested additional nurses in 2022 and 2023, but administrators did not approve the increase.
Safe-Staffing Petition Signed Days Before the Fatality
In the days leading up to December 8, 2023, nearly all ER nurses signed a petition requesting safe staffing. The fatality occurred while signatures were still being gathered.
Dr. Chew Warned, “Bad Things Could Happen.”
During the CMS investigation of Francisco’s death, Kaiser Vallejo ER physician Gordon Chew admitted to investigators that low staffing and the failure to escalate the issues resulted in Francisco’s death. He said ESI Level 2 patients (Francisco) should have been reassessed every two hours. But the physician’s testimony was ominous: “If nursing was short-staffed and the emergency room was full, bad things could happen!”
CEO Greg Adams Denied Staffing Problems to State Investigators (Jan 10, 2024)
…” staffing had never been an issue… complaints of short staffing were from a bad night they [nurses] experienced.”

On January 10, 2024, a month after Francisco’s death, the CEO spoke to state investigators acting on behalf of CMS. The CEO had 4 weeks to be briefed on the facts of the case by his staff. The CEO was interviewed briefly by investigators. The report included quotes from the CEO.
- “He stated staffing had never been an issue.”
- In addition, “He stated he spoke with staff and usually the complaints of short staffing were from a bad night they [nurses] experienced.”
Yet, in formal written complaints, the Kaiser Vallejo ER nurses repeatedly reported staffing was a perilous issue. The CMS Summary Statement of Deficiencies verified that staffing was an issue. “There was not enough emergency room staff to provide effective emergency care when patients were not assessed and monitored.“
The CEO’s statement that “staffing had never been an issue” was untrue. Staffing was an issue. It was previously documented in a 2021 CMS deficiency report detailing staffing failures at this Kaiser ER. In 2023, Mr. Adams’ compensation was listed at $17,268,060. Patient safety may not have been a top priority for Mr. Adams.
Oversight Failures at Governing-Body Level
Under federal regulations, the hospital’s governing body is responsible for ensuring safe and effective care. In its findings, the CMS Summary Statement of Deficiencies concluded that Kaiser Permanente’s Governing Body failed to meet required oversight responsibilities in relation to the Kaiser Vallejo ER. The CEO, Greg Adams, also served on the Governing Body.
Physicians on Governing Body Failed To Provide Needed Oversight
The Kaiser Governing Body included three physicians with nationally recognized credentials:
- Richard Shannon, MD — Chief Medical Officer, Duke University Health System
- Regina Benjamin, MD — 18th U.S. Surgeon General
- A. Eugene Washington, MD — Chancellor Emeritus, Duke University
According to CMS, these members, along with other Governing Body members, did not provide the level of oversight required by regulation for emergency department operations and patient monitoring.
Governing Body Compensation (over $250,000 per year)
10 of 13 Governing Body members have a business or legal background. Thus, the Governing Body is heavily weighted for business planning and financial oversight, rather than oversight of Kaiser’s mission to provide “high-quality” healthcare. Moreover, the Board members receive generous compensation for attending meetings. The average annual compensation for each member of this Kaiser Governing Body was over $250,000, according to Kaiser’s federal tax returns for 2023.
Kaiser Reported $4.1 Billion in 2023 Net Income

Top Row: Greg Adams, Ramon Baez, David Barger, Regina Benjamin, MD, Jeff Epstein, Leslie Heisz. Bottom Row: David Hoffmeister, Judith Johansen, JD, Jenny Ming, Matthew Ryan, Richard Shannon, MD, Vivek Sharma. (A. Eugene Washington, MD, was mistakenly left off the image above.)
Arbitration Filed for Francisco’s Family by Mitchell Leeds, LLP

On behalf of Francisco’s family, a San Francisco medical malpractice attorney, Nathaniel Leeds, is pursuing arbitration with Kaiser. Mr. Leeds, the son of a doctor, learned at an early age the importance of quality medical care and the needless harm patients and their families incur when a healthcare system fails them.
“We’ve probably done over a hundred cases of malpractice that arose in emergency rooms. Emergency rooms are where healthy people go when something has happened that is emergent. When doctors and nurses treat patients well, emergency rooms are amazing places. They take you from a place where you are potentially going to die, and you can walk out living a normal life. But when things go badly, people end up horribly injured in emergency rooms. I’ve represented a lot of folks harmed in an emergency room. We continue to have that as a significant part of our practice.
Hospital Watchdog welcomes comments and suggestions.
Kaiser Permanente Vallejo Medical Center, Photo by Gretchen Zimmerman


No comments yet. Be the first to comment!