
By Rachel Nurudeen & Bob Aller
September 13, 2025
Hospital ER staff cruelly denied care for a mother in preterm labor, causing a traumatic, tragic birth outside the hospital in the front seat of a car.
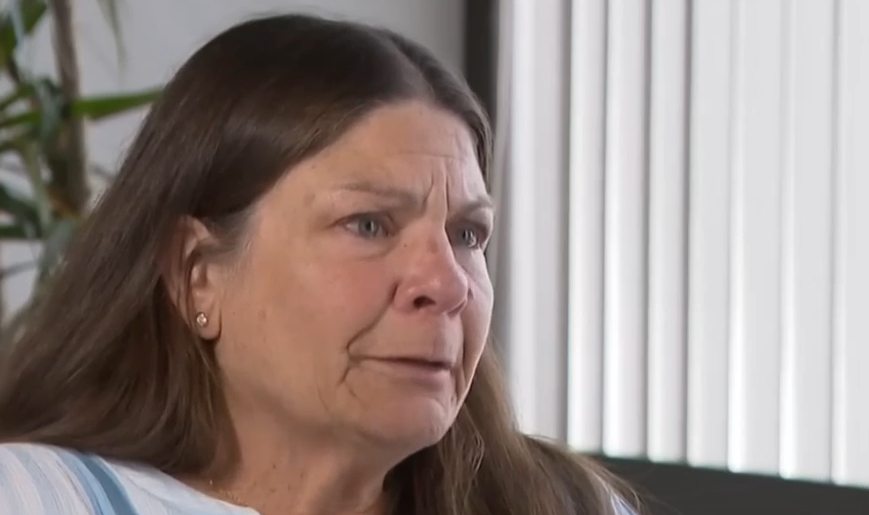
The mother, Hannah Michaelis, had dreamed of becoming a mother for as long as she could remember.
At 29, that dream was finally coming true. Hannah was pregnant.
She was living in rural Tennessee with her partner, Samuel Vorenkamp. Her mother, Carla Michaelis, lived in El Cajon, a suburb of San Diego. Worried about Hannah’s access to excellent prenatal care, Carla encouraged her daughter to come home and stay with her during her pregnancy. In March 2024, Hannah flew home.
Pregnancy Required ER Visits

At 23 weeks, on May 4, 2024, Hannah experienced troubling cramping and pain. She received emergency care at the Sharp-Grossmont Hospital ER in La Mesa, California. But she was discharged home from the ER, despite worrisome symptoms.
That night, the symptoms got worse. The next day, Hannah was experiencing severe cramping and sharp abdominal pains. Fearing preterm labor, her mother promptly drove her back to the Sharp-Grossmont Hospital ER, just minutes from their home. The ER claimed it was the largest ER in East San Diego County… “We’ll safely get you the 24-hour emergency care you need.”
An ER Nurse Stated The ER Couldn’t Treat Hannah Since She Was In Active Labor
Carla reported that upon arrival, an ER nurse refused to provide ER services for Hannah. She said since Hannah was in active labor, they couldn’t see her. Carla pleaded for the staff to take care of Hannah. Instead, the ER nurse directed Carla to go to the University of California at San Diego hospital, 30 minutes away by car. But since her daughter was in labor, Carla thought the drive would be unsafe and ill-advised.
Was “Active Labor” The Real Reason For Denial Of Care?
Though hospital staff said they couldn’t treat Hanna because she was in active labor, the ER reports that it sees around 300 patients each day. Additionally, the separate on-campus Sharp-Grossmont Hospital for Women and Newborns had a 24-bed Neonatal Intensive Care Unit (NICU). The ER staff was acutely aware that Hannah’s baby would be preterm, requiring intensive care in a NICU. Even so, they denied Hannah the emergency care she desperately needed for the birth.
Violation Of EMTALA
By refusing care to a woman in labor, the intake staff at the Sharp-Grossmont ER appears to have violated the federal Emergency Medical Treatment and Labor Act (EMTALA). The law requires hospitals to screen and stabilize those who enter an emergency department seeking care. No exceptions are allowed.
CMS regulations even require Emergency Departments to post signs outlining patients’ rights under EMTALA. EMTALA is no secret. When Hannah was denied care, the ER staff showed a reckless disregard for the safety of a 23-week preterm baby.
However, with lax federal enforcement of EMTALA, some hospitals violate EMTALA for cost-saving or other reasons.
Posts in a nurses’ Reddit forum on this case suggest EMTALA may have also been violated for other patients.
“…We had to take several clients to Grossmont ER only for them to turn them around and tell them they had to go to another ER due to insurance issues.”
“The only hospital that could regularly be counted on to try to tell me I couldn’t bring them there was Sharp Grossmont…Not surprised to see something like this happen there. So tragic for that mom and her baby.”
—————————————————————————————————————————-
Hannah and her mother left the ER. Carla called 911 seeking an ambulance for safe transportation to the University of California at San Diego Hospital. Unfortunately, she was told that 911 emergency services couldn’t help her. Frustrated, she hung up.
Concerned about the circumstances of a woman in labor, the 911 dispatcher called the ER. She spoke with a nurse who sounded annoyed by Carla’s frustration over the ER’s refusal to provide care.
Birth Occurred In The Car

If a 23-week infant (an extremely premature, “micro-preemie”) is born outside a hospital without medical care, the literature indicates the birth almost always results in the death of the baby. The infant is on the threshold of viability. Lungs cannot function without mechanical support. Brain blood vessels are prone to severe intraventricular hemorrhage. An incubator is required to manage body temperature. Those infants who do survive a birth without intensive medical care usually succumb within hours or days due to respiratory failure, hypothermia, or brain hemorrhage.
After Hannah was denied care by ER staff, she and her mother returned to their car in the parking lot. Hannah gave birth at 23 weeks in the front seat.
Carla: “It happened fast. There was blood all over the seat. Her water had broken in the front seat of my car. She said something else is wrong, Mom. I put my hand in my pants, and I could feel his body.”
Hannah delivered the baby without the intensive medical care required to protect the extreme fragility of a 23-week-old baby.
Right after the birth, a nurse from the ER arrived with a wheelchair. Carla and Hannah recalled the nurse rolling her eyes in disbelief when they told her the baby was born into Hannah’s underwear. Without checking to see if Baby Samuel was in Hannah’s underwear, the nurse transferred Hannah from the front seat of the car to a wheelchair. The jostling during the wheelchair ride had to be traumatic for an extremely vulnerable infant, on the edge of survivability.
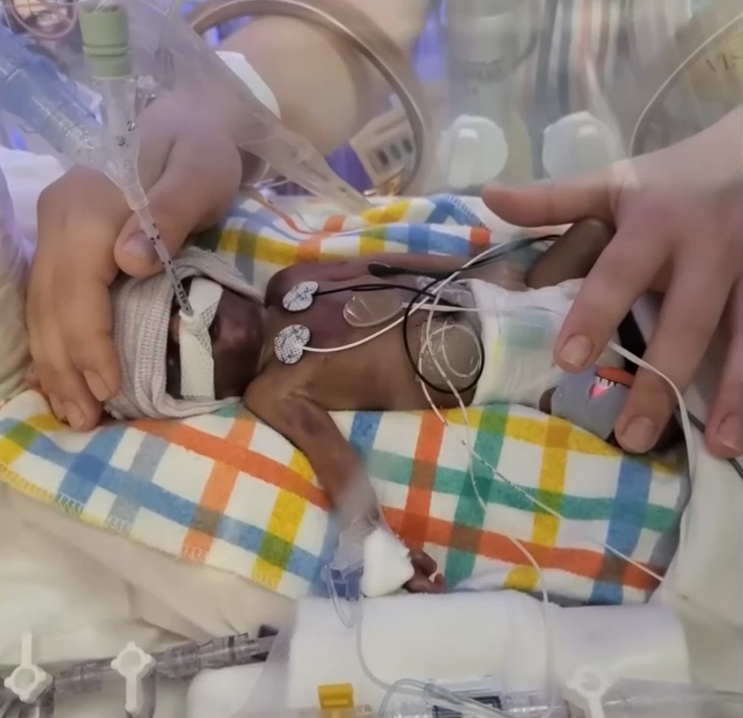
Baby Samuel Suffered Trauma
EMTALA requires that the ER stabilize the infant to the extent possible. Baby Samuel was transferred to the NICU at the on-campus Sharp Hospital for Women and Newborns. Baby Samuel had pronounced bruising around the head, shoulders, and neck. Tests would show he suffered two severe intraventricular brain hemorrhages. Most hospitals require staff to immediately notify the Risk Manager about potentially fatal adverse events. Most hospitals have Risk Managers promptly prepare reports on such incidents by interviewing those who provided care. In this case, the NICU physicians were Drs. Wozniak and Rasmussen. Five days later, on May 10th, Baby Samuel was pronounced dead at 10:43 AM.
📋 CMS Transfer Documentation Requirements
Under CMS regulations (42 CFR §489.24(e), when the Sharp-Grossmont ER staff transferred Baby Samuel to the NICU, the ER was required to provide the patient’s medical records, including the history related to the emergency condition. This documentation is required for transferring the patient and for billing purposes. Baby Samuel’s birth in the car was critical information to be provided to the NICU physicians, Drs. Wozniak and Rasmussen.
Comments From Staff At Another NICU
Hospital Watchdog contacted staff at another NICU for their comments on this case. The staff spoke under the condition of anonymity.
A Registered Nurse Certified in Neonatal Intensive Care: “Refusing immediate care to a mother in labor at 23 weeks essentially eliminates the baby’s chance of survival.”
The female head of the NICU: “At 23 weeks, a delivery in an automobile and outside a hospital makes a catastrophic brain hemorrhage much more likely.”
A neonatologist: ” A traumatic delivery outside a hospital exposes the premature baby to hypoxia (insufficient oxygen) and mechanical stress (physical forces that can damage the brain), further worsening an already poor prognosis and likely resulting in fetal demise.”

Carla: “They decided to take him off of everything except for his intubation tube so Hannah could have skin-to-skin contact with him until he stopped breathing.”
NICU Physician Created A Death Report That Omitted Baby Samuel’s Traumatic Birth

When a patient dies in a hospital, a physician writes a Report of Death (a summary of the causes of the death). The Report of Death, a medical record, is source material for the Death Certificate.
However, when adverse events or medical negligence occur, some doctors knowingly shield their employer by omitting key facts that might subject the hospital to legal liability. But under federal regulation 42 CFR §482.24, all entries in medical records must be complete. Under CMS enforcement practices, the omission of material facts in medical records is considered a form of falsification. An incomplete record is misleading. The record fails the regulatory requirement for accurate and complete medical records.
In this case, a profoundly significant, well-established fact was omitted from the Report of Death. Baby Samuel experienced a traumatic birth.
According to Dr. Wozniak, Baby Samuel died solely from natural causes. The “severe prematurity” triggered severe bleeding and pressure on the brain. Dr. Wozniak’s report, omitting the traumatic birth, cleared a legal hurdle for the hospital. The hospital would claim it was not liable for damages since the baby died solely from natural causes.
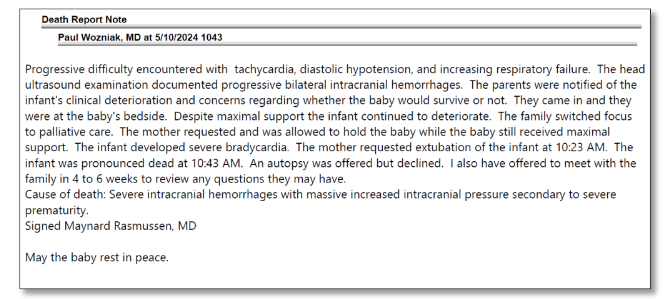
Maynard Rasmussen, MD, signed the death report. His signature confirmed his full agreement with Dr. Wozniak’s report. Dr. Rasmussen had served on the Medical Executive Committee and other committees serving the hospital’s interests. Together, these physicians, by omission, appear to have covered up material facts related to the death of Baby Samuel.
Dr. Rasmussen Completed The Death Certificate But Omitted Traumatic Birth & Associated Injuries

California Health & Safety Code §102875 requires the attending physician (or other authorized certifier) to state the direct cause of death, including other significant conditions such as an antecedent cause of death and an injury. Such secondary conditions must be listed on a death certificate. But the traumatic birth and associated injuries were omitted.
NICU staff interviewed at another NICU facility stated that a traumatic birth outside a hospital would have a profound impact on the survivability of a 23-week infant. The Neonatal Research Network (NRN) previously reported a survival rate of about 32% for infants born at 23 weeks—this improved to 49% for a more recent cohort when aggressive treatment was provided
But infants born at 23 weeks and receiving no medical care at birth have a survival rate of virtually 0%.
Consider The Conduct of the Caregivers! First, Care For A Mother In Labor Is Denied. After Causing A Tragic Event, Caregivers Claim In A Legal Filing That They Are Not Responsible, In Any Way, For The Fatality That Followed. 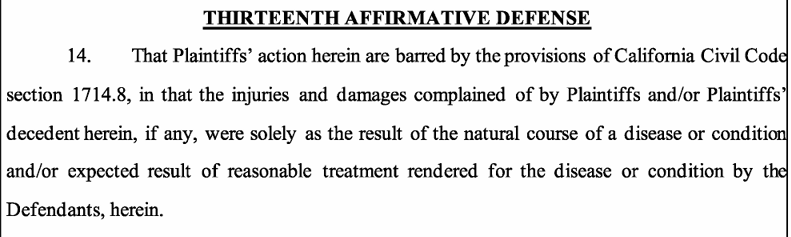
Hospital’s response to plaintiff’s amended complaint

The law firm of Ikuta Hemesath, LLP, represents Hannah and Carla Michaelis.
Attorney Janna Trolia described what should have happened. “If Hannah had been immediately triaged and brought into a labor and delivery suite or operating room, rather than left to give birth alone in her underwear outside the labor unit, Baby Samuel would have received life-saving interventions the moment he was born. We find it profoundly disturbing that Grossmont staff mocked and ridiculed Carla as she pleaded for assistance…”

No comments yet. Be the first to comment!