Bishop Jaime Soto — Responsible For Implementation Of Catholic Teachings At Dignity Health’s Mercy San Juan Medical Center
By Robert Aller, Dec 11, 2025
The National Conference of Catholic Bishops adopted the Ethical and Religious Directives for Catholic Health Care Services (ERDs) in 1971. These Directives became the ethical and religious standards for all Catholic healthcare facilities. At Catholic hospitals, “the diocesan bishop has the responsibility to ensure the moral and religious identity of the health care ministry in his diocese.”
At Mercy San Juan Medical Center in the Greater Sacramento Area, California, Bishop Jaime Soto is responsible for ensuring Catholic moral teachings are implemented. Dignity Health, the largest hospital chain in California, owns this hospital and five others in the area. But Bishop Soto retains the authority to grant, maintain, or withdraw Catholic identity.
However, under Bishop Soto’s jurisdiction, repeated state investigations revealed that Dignity’s Mercy San Juan staff violated state laws regarding the deceased. Hospital staff, including physicians, were involved in flagrant transgressions of the ERDs and Catholic teachings. This conduct led to the advanced decomposition of human remains stored for years in an off-site facility.

California Department of Public Health Conducted 3 Investigations On Handling Human Remains At Dignity’s Mercy San Juan Medical Center
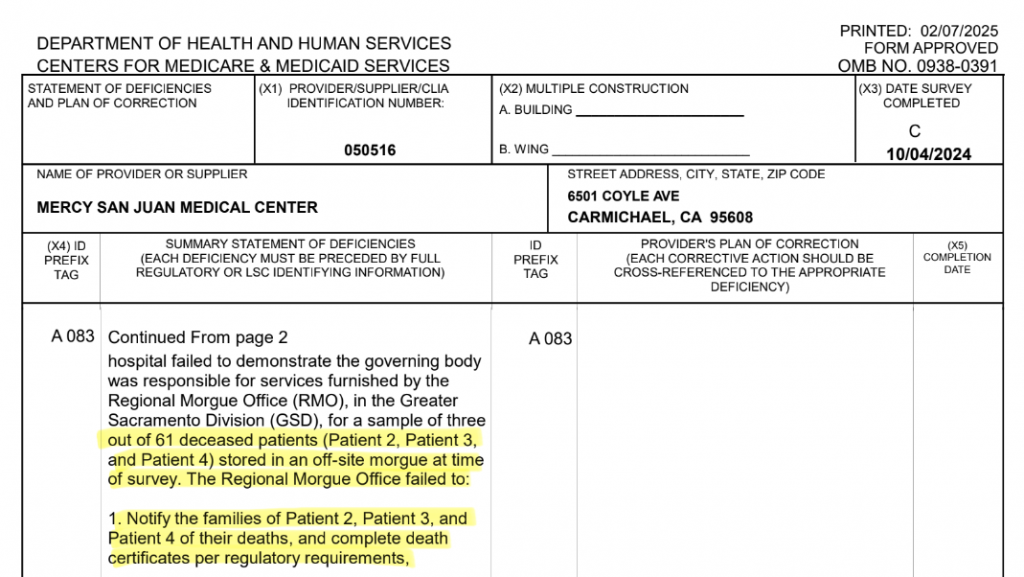
The California Department of Public Health (CDPH), acting on behalf of the Centers for Medicare & Medicaid Services (CMS), conducted investigations in 2022, 2023, and 2024. In each investigation, the state surveyors found egregious handling of human remains.
Desecration Of Mercy San Juan Patients
Desecration is the act of depriving something of its sacred character, or the disrespectful, contemptuous, or destructive treatment of that which is held to be sacred or holy by a group or individual. (Wikipedia)
Catechism of the Catholic Church (CCC 2300):
“The bodies of the dead must be treated with respect and charity, in faith and hope of the Resurrection. The burial of the dead is a corporal work of mercy; it honors the children of God, who are temples of the Holy Spirit.”
Findings In CMS Deficiency Reports:
- After patient deaths, no death certificate was completed by a physician, in violation of state law.
- No next of kin was notified of the death, in violation of state law.
- No death certificate was filed with the state registrar, in violation of state law.
- Without a permit, in violation of state law, bodies were shipped to an off-site storage facility.
- Human remains were stored for years, reaching advanced states of decomposition, in violation of state law.
Dignity’s Mercy San Juan Breached Its Agreement To Correct Violations of State and Federal Law
When the CMS Summary Statements of Deficiencies were issued in 2022 and 2023, the hospital assured the state that the problem would be corrected. However, in 2023 and 2024, investigators found the hospital failed to correct the violations of state regulations.
During the 2024 inspection, a hospital supervisor testified she repeatedly escalated concerns about unfiled death certificates to regional leadership (Dignity Health) and the hospital president (Michael Korpiel), but “it went nowhere.” (Dignity Health is one of the largest health systems in the U.S. with 400 health care sites, including 39 hospitals — 24 are Catholic. Revenue for 2024 was 11.3B.)
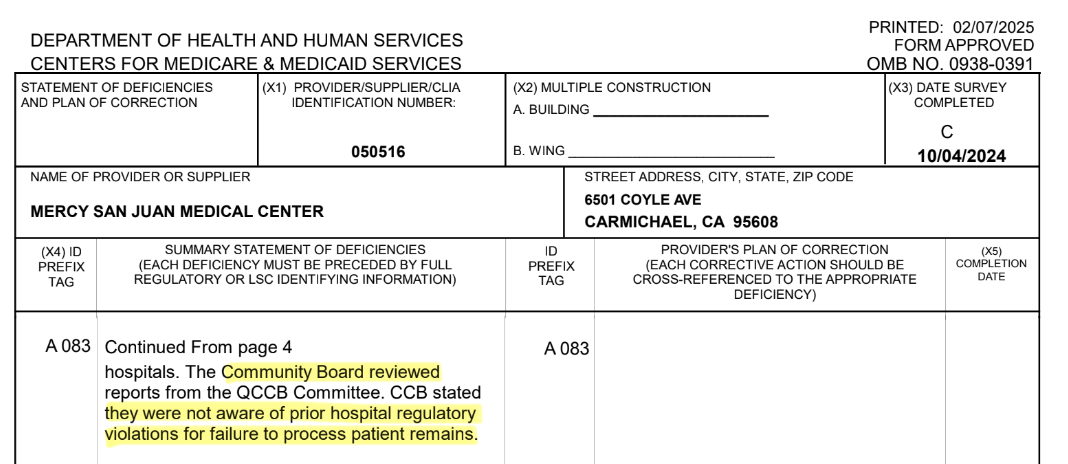
Dignity’s Mercy San Juan Staff Violated Federal Law By Concealing Regulatory Violations From Its Governing Board
42 CFR §482.12 – Condition of Participation: Governing Body

Under federal law, CMS requires that a hospital’s governing body be kept informed of regulatory violations, compliance problems, and deficiencies identified by state survey agencies. But the egregious regulatory violations were concealed from the Governing Board. Sister Nora Mary Curtin, a member of the hospital’s founding Sisters of Mercy Order, served on the governing board. (In Sacramento, Dignity’s governing board is called the Community Board.) But hospital administrators concealed the regulatory violations from Sister Curtin and the other Board members.
Sisters Of Mercy’s Core Beliefs Discarded

The Sisters of Mercy were founded in Dublin, Ireland, in 1831. They believed that every human being—living or deceased—possesses inherent dignity that demands truthfulness, reverence, and respectful care. They founded this hospital in 1967. Their charism holds that the body, even after death, remains a sacred vessel that must never be hidden, neglected, or allowed to deteriorate without proper burial. Mercy institutions have emphasized honoring the dead, especially the poor and forgotten, as a core moral duty. Not true here.
Bishop Soto Remains Publicly Silent!
With ERD Directives 70 & 71, leaders of Catholic hospitals are obligated to consult with the local diocesan bishop promptly if there are immoral activities or risk of a “scandal.” In this case, the hospital was already in an immoral and active scandal with local, national, and international news reports of the case, but Bishop Soto remained publicly silent. (Hospital Watchdog contacted the Sacramento Diocese to speak with Bishop Soto or any other diocese staff about the case. However, the diocese was non-responsive to multiple requests.)
Hospital CEO: “We Assumed The Remains Being Stored Did Not Have Families”
The core question of “Why” was addressed in testimony from Michael Korpiel, CEO of Mercy San Juan Medical Center at that time. In 2024, he spoke to investigators from the California Department of Public Health. “We assumed the remains being stored did not have families,” he said. The CEO explained that the patient populations at the hospital included high numbers of homeless persons. However, living apart from family did not warrant disrespect for the bodies of the deceased. When asked to explain the lack of oversight on the problem, the CEO stated that the issue would be addressed at the divisional level (Dignity Health), “It is not my scope.”
Catholic moral law views obscuring the truth as a violation of moral obligations toward truth and justice.
Documented Tracked Its Mishandling Of Human Remains
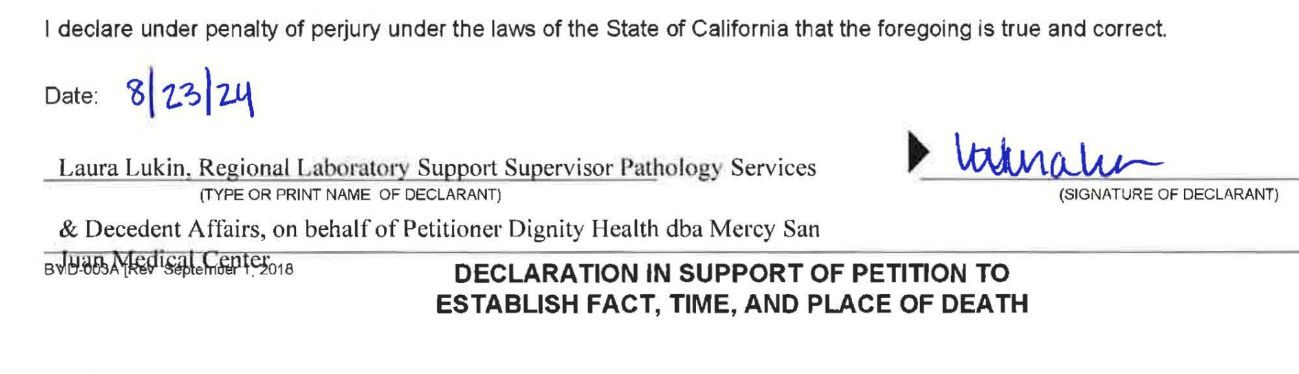
Data from this Dignity Hospital’s post-mortem set of reports revealed administrative conduct allowing the ongoing mishandling of human remains for a sub-group of 100 patients. (There are more than 100 deceased who were mishandled.)
Mortuary Support Services of Northern California (contracted by Dignity to store human remains) sent frequent notices to Dignity’s Supervisor of Decedent Affairs, Laura Lukin.
The notices reported the status of human remains in storage from four Dignity hospitals in Bishop Soto’s Sacramento diocese: Mercy San Juan Medical Center, Mercy General Hospital, Methodist Hospital of Sacramento, and Mercy Hospital of Folsom. A total of 100 patients appear in these records.

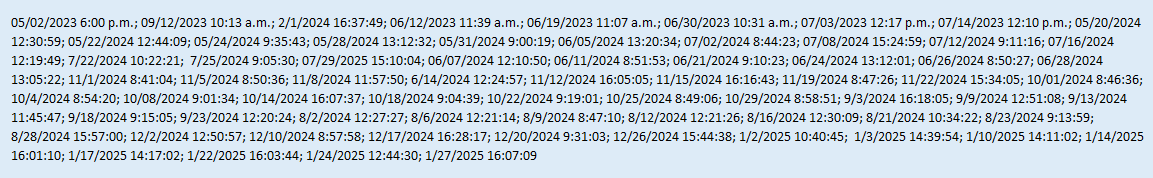
For just one deceased patient, over two years, Ms. Lukin received 69 overdue notices. Each notice reminded Ms. Lukin that the patient’s death certificate—required by California law to be filed within ten days—had not been filed.
These notices were sent frequently. Yet, human remains were stored for years. In total, Ms. Lukin received over 2,800 overdue death certificate notices for 100 patients. As a Dignity Health hospital administrator, Ms. Lukin disregarded the ERDs along with provisions of the California Health and Safety Code and federal regulations.
69 Notices Of No Death Certificate For One Patient 05/22/2023 – 1/27/2025
Case Example: Jessie Peterson

On April 6, 2024, Jessie Peterson, 31, was admitted to Dignity Health’s Mercy San Juan Medical Center ER. At age 10, she was diagnosed with type 1 diabetes. In recent years, she had been hospitalized numerous times for severe diabetic episodes. Jessie had struggled with substance abuse and was living in a shelter, and alternately with friends. Yet, despite the instability in her life, Jessie remained closely connected to her sisters and mother. In her hospital records, Jessie’s mother was listed as her primary contact.
When Jessie arrived in the ER, she was experiencing a severe diabetic episode. She was transferred to the ICU. A central line was placed in Jessie. (Over 5 million central lines are placed each year in the U.S.) A central line is a long, flexible catheter placed into a large vein to deliver medications, fluids, or nutrition, draw blood, and monitor critical pressures in seriously ill patients.
But two days later, on April 8th, Jessie was alert and doing much better. The central line was no longer needed. She was moved to a Med Unit, a step down from the ICU. But the state investigators found that the hospital had not followed hospital policy and removed the central line while Jessie was in the ICU, before Jessie was moved. The central line was removed in the Med Unit. But right after the central line was removed, Jessie suffered a fatal cardiac arrest, though she had been doing much better.
Fatal Cardiac Arrest Can Result From Negligent Removal Of Central Line
Hospitals have a strict policy for removing central lines. If the policy is not followed, air can be sucked into the vein because of the negative pressure in the chest during breathing. An air embolism can quickly block blood flow, causing a sudden drop in blood pressure followed by cardiac arrest. This adverse event is considered a Sentinel event. If Jessie’s central line had been improperly removed by staff, the removal would constitute medical malpractice. (It is estimated that there are about 1,500 fatalities resulting from air embolisms in the U.S. each year. A significant percentage of these air embolism fatalities are linked to central line issues.)
Sacraments of Initiation
On the day that Jessie died, her mother, Ginger Congi, received the Sacraments of Initiation into the Catholic Church. But no one from Dignity’s Mercy San Juan ever contacted Jessie’s mother to inform her of Jessie’s passing and to provide pastoral care.

According to the American Medical Association’s Principles of Ethics, “informing a patient’s family that the patient died is a fundamental duty in the patient-physician relationship.” Yet, Jessie’s doctor, Nadeem Muktar, never contacted Jessie’s mother to tell her Jessie had died. The hospital later claimed that staff called Jessie’s mother, but didn’t leave a message since it would violate HIPAA. The hospital should have known that leaving a message to return a phone call does not violate HIPAA!
Dr. Muktar completed Jessie’s death certificate a year after Jessie’s death. Why would Dr. Mukhtar fail to complete Ms. Peterson’s death certificate within 15 hours as required by law?
Jessie’s Mother Was Told Jessie Left The Hospital Against Medical Advice
On April 12th, Jessie’s mother called Mercy Hospital to check on Jessie’s progress. She was told that there was “no one here by that name.” After insisting on more information, she was told that Jessie “left against medical advice.” Hospital staff did not disclose that Jessie died four days earlier. Staff failed to disclose that Jessie’s remains had been moved to an off-site storage facility.
Convinced that Jessie was a missing person, Jessie’s mother and her sisters, Angie and Chandra, embarked on an intensive year-long search. The family filed a missing person report with the Sacramento County Sheriff’s Office. Jessie’s information was posted on the Department of Justice website for missing persons.

In their search for Jessie, the family showed her photo to many homeless people. For one long year, they never stopped looking. Finally, they were notified by a Sheriff deputy that Jessie’s remains had been located at a storage facility.
By that time, a year after her death, her remains had decomposed. She was no longer recognizable. An autopsy or an open casket funeral was not possible. No one from Mercy San Juan ever contacted the family to offer pastoral care. Later, a lawsuit was filed in the Superior Court of Sacramento on behalf of Jessie Peterson’s family.
Case Example: Tonya Walker

On October 31, 2023, Tonya Walker was admitted to another Dignity Health hospital in Sacramento. At Mercy General Hospital’s ER, Tonya’s medical records cited extremely low blood sugar, high blood pressure, and elevated potassium levels. Though Tonya also struggled with homelessness, she provided the hospital with family contact information. She registered as Catholic. She did not consent to organ donation.

On November 2, 2023, at 3:11 a.m., Ms. Walker suffered a fatal heart attack and was pronounced dead by attending physician Andrew Norris. But Dr. Norris, nor any other doctor, completed the death certificate as required by California law. What would motivate Dignity doctors to violate state law and fail to complete Ms. Walker’s death certificate? In California, death certificates are completed online via the California Electronic Death Registration System (CA-EDRS). The law requires completion within 15 hours. The death certificate is then routed to the local registrar. Studies show it only takes a few minutes for a doctor to fill in key medical information.
After Tonya’s death, no doctor or hospital staff contacted Tonya’s family to let them know Tonya had died, and to offer pastoral support.
Ms. Walker’s remains were shipped in a body bag to the same off-site storage facility where Jessie Peterson’s remains were stored. Tonya’s remains were also left to decompose, alongside the remains of many others.
By sending Ms. Walker’s remains off-site without family notification and lawful authorization, Mercy General abandoned its sacred obligation to treat the body as the former dwelling place of the soul, a violation of Catholic moral teaching on human dignity after death.
Tonya Walker had always maintained contact with her family. When she suddenly stopped responding, the family launched a search. Assuming she was a missing person, the Sacramento Sheriff was notified. The family distributed flyers throughout Sacramento, posted digital notices on social media, and offered a $3,500 reward.
Tonya’s sisters combed the streets and posted flyers in areas where they knew Tonya frequented. They even had to deal with the circumstances of someone claiming Tonya was being held for ransom.
On May 31, 2024, after seven months of searching, a Sheriff’s deputy called and told the family Tonya had been found on a shelf in a storage facility in South Sacramento. The sisters went to the facility that same day.
“They tried to convince us not to see her. But we weren’t going anywhere,” said Tonya’s sister, Dalee.
Although Catholic hospitals do not charge for viewing, the storage facility charged Kalia and Dalee $250 to view their sister’s remains.
When the cover was lifted, Tonya’s remains lay in an advanced state of decomposition. From what they saw, her eyes were gone. It appeared her eyes had been taken, raising the possibility of organ theft. Upon admittance, Tonya had not consented to be an organ donor. Did organ trafficking occur?
According to a sister, parts of Tonya’s skin were also missing. Tonya could only be identified by the portion of a tattoo on her arm.
No one from Mercy San Juan ever contacted the family. A lawsuit was filed in the Superior Court of Sacramento County on behalf of Tonya Walker’s family.
Hospital administrators and staff, by their statements, actions, and failure to correct the deficiencies, demonstrated they were not adequately committed to “following the teachings of the Catholic Church.”
Unsubstantiated Claim: Hospital Administrator Laura Lukin Blames Lengthy Storage Of Remains Of Charles Harvey Due To COVID-19 & Staffing Issues
An explanation for the delay in writing a death certificate for the deceased patient, Charles Harvey, was provided in a court petition filed by the Supervisor of Deceased Affairs, Ms. Laura Lukin. Ms. Lukin attributed a two-year delay to COVID-19 and staffing issues. (There is no indication that any of the patients placed in storage had died from COVID-19.)
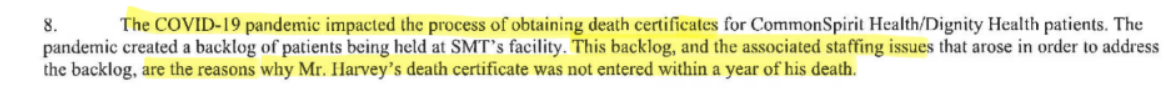
Ms. Lukin filed a petition for “An Order Establishing Fact of Death” to be used in place of a death certificate. Mr. Harvey died on June 21, 2022. Ms. Lukin took over two years, until August of 2024, before she took action.
No Evidence Indicates COVID-19 & Staffing Issues Caused Maltreatment Of The Deceased
There are no public records found from the time of Mr. Harvey’s death indicating that COVID-19 was delaying the processing of human remains and death certificates for other hospitals in Sacramento.
Ms. Lukin claims there were staffing issues. However, California Health and Safety Code regulations provide that when the attending physician is unavailable, another physician can complete a death certificate. If no other physician is available, the coroner or medical examiner can complete and sign the death certificate.
Mercy San Juan staff failed to provide a credible explanation for its conduct. Mercy’s explanation for its conduct appears to be patently untrue.
Mercy San Juan Is The Only Hospital In The U.S. With CMS Reports Of Storing Human Remains For Years!
Dignity Health’s Mercy San Juan appears to be the only hospital in the United States where CMS investigations found the hospital had stored large numbers of bodies in body bags for years.
It appears Mercy San Juan is the only hospital in the U.S. that has claimed COVID-19 and staffing issues forced the hospital to store a large number of human remains unlawfully for years. Implicit in the hospital’s claim is that COVID-19 and staffing issues rendered the hospital unable to notify next of kin of a death and unable to complete death certificates.
Why did Mercy San Juan permit the unlawful, non-notification to families of the death of a loved one?
Why did Mercy San Juan permit the unlawful non-completion of death certificates by doctors?
Why did Mercy allow bodies to be stored unlawfully for years in a storage facility while they decomposed?
Will Bishop Soto Permit A Catholic Church To Continue To Deceive The Public?
The Sacramento public deserves to know the absolute truth. Nearly 20,000 patients are admitted to Mercy San Juan Medical Center each year. Only through real transparency can the Sacramento Diocese and Dignity’s Mercy San Juan Hospital honor the dignity of those desecrated by Mercy San Juan’s staff.
Catholic moral theology, detailed in canon law and other Catholic teachings, requires that a Catholic facility be truthful in all its communications. Yet, Dignity Health has provided an untruthful explanation.
However, when ERDs are violated, some Bishops have revoked Catholic status for hospitals.
Bishops Can Remove Catholic Status

In 2010, Phoenix Bishop Thomas Olmsted declared St. Joseph’s Hospital and Medical Center—then part of Catholic Healthcare West, the same corporate lineage that became Dignity Health—could “no longer be called a Catholic hospital.” After a disputed abortion and broader ERD violations, he ordered the removal of the Blessed Sacrament and prohibited Mass on site. In Oregon that same year, Bishop Robert Vasa revoked the Catholic status and sponsorship of St. Charles Medical Center in Bend, run by a non-religious nonprofit corporation, after the hospital continued performing sterilizations contrary to the ERDs. In both cases, the bishops did not own the hospitals, did not control their boards, yet they severed the Catholic identity.
Bishop Jaime Soto has the canonical authority to revoke the hospital’s Catholic status—and other Bishops have already done so for corporate-owned hospitals.
What Is Bishop Soto’s Position?

#67. “Each diocesan bishop has the ultimate responsibility to assess whether collaborative arrangements involving Catholic health care providers operating in his local church involve wrongful cooperation, give scandal, or undermine the Church’s witness…”
Although the Church has condemned violations of certain ERDs at other hospitals, Bishop Soto has remained conspicuously silent regarding extensive violations of ERDs and Catholic teachings meant to protect the deceased. Why?
Unthinkable Conduct
For years, Dignity’s Catholic Mercy San Juan Medical Center engaged in unthinkable conduct—disregarding the Ethical and Religious Directives and core teachings of the Catholic Church related to the deceased. Documents reveal that the scale of this unthinkable conduct involves at least 180 patients from 5 Dignity hospitals, along with their families and loved ones. The Sacramento Diocese, by its silence, has shown no objections to the hospital’s past egregious conduct. By its continuing silence, the Sacramento Diocese appears to allow the hospital to conceal, with untruthful claims, how and why these sacrilegious acts on human remains were carried out under its Catholic name.
PARTIAL LIST OF HUMAN REMAINS

Decedent Affairs Supervisor Raises Concerns
Hospital Watchdog shared the details of this case with a Decedent Affairs supervisor at another hospital of equal size. The supervisor, highly experienced with decedent issues, raised possibilities. “The repeated failure to inform the next of kin of these patients is deeply concerning. It raises the possibility of deliberate concealment. It also raises the question of whether decomposition served a strategic purpose.” ###

No comments yet. Be the first to comment!